Global health correspondent
 Ghetto images
Ghetto imagesIt is estimated that more than three million children worldwide were killed in 2022 as a result of antibiotic -resistant infections, according to a study by two leading experts in the field of child health.
Children in Africa and Southeast Asia have been found to be at risk.
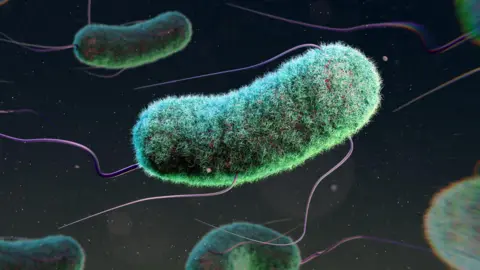
Antimicrobial resistance – known as AMR – develops when the germs that cause infections develop in such a way that antibiotic drugs no longer work.
It is identified as one of the largest threats to public health that the world's population faces.
A new study now reveals the fee AMR accepts children.
Using data from multiple sources, including the World Health Organization (WHO) and the World Bank, the authors of the report estimated that more than three million children of children associated with drug resistant infections were linked in 2022.
Experts say this new study emphasizes more than a tenfold increase in AMR -related infections in children in just three years.
The number could be worsened by the effects of the Covid pandemic.
Increased use of antibiotics
Antibiotics are used to treat or prevent a huge set of bacterial infections – all from skin infections to pneumonia.
Sometimes they are also used as a precautionary measure to prevent, not treatment, infection – for example, if one has surgery or receives chemotherapy cancer treatment.
Antibiotics do not affect viral infections, although diseases such as common cold, flu or cavides.
But some bacteria have now developed resistance to some medicines due to their excessive use and inappropriate use, while the production of new antibiotics – a long and expensive process – slowed down exactly down.
Leading authors of the report, Dr. Janhong Jessica Hu, of the Murdoch Children's Research Institute in Australia and Professor Herb Haruel of the Clinton Health Initiative, point to significant growth in the use of antibiotics that aim to be restrained only to the most serious infections.
Between 2019 and 2021, the use of “observed antibiotics”, high -risk drugs, increased by 160% in Southeast Asia and 126% in Africa.
During the same period, “reserve antibiotics” – treatment with the last time for severe, multi -resistant infections – increased by 45% in Southeast Asia and 125% in Africa.
Plastering options
The authors warn that if bacteria develop resistance to these antibiotics, there will be few, if any, alternatives to treat multi -resistant infections.
Prof. Harwell presents the discoveries of the Congress of the European Society of Clinical Microbiology and Infectious Diseases in Vienna later this month.
“AMR is a global problem. It affects everyone. We have done this job really to focus on the disproportionate way AMR affects children,” he said before the event.
“We appreciate three million deaths of children worldwide related to antimicrobial resistance.”
Is there a solution for AMR?
WHO describes AMR as one of the most serious global health threats We are confronted, but speaking from Vienna, Prof. Harwell warns that there are no easy answers.
“This is a multifaceted problem that extends into all aspects of medicine and indeed, a human life,” he said.
“Antibiotics are ubiquitous around us. They find themselves in our food and the environment, and so inventing a solution is not easy.”
The best way to avoid resistant infection is to completely avoid the infection, which means that higher levels of immunization, water sanitary and hygiene are needed, he adds.
“There will be more antibiotics because there are more people who need them, but we need to be sure that they are appropriately used and the right medicines are used.”
Dr. Lindsay Edwards, a senior microbiology lecturer at King's College London, said the new study “marked a significant and anxious increase compared to previous data.”
“These findings should serve as awakening for global health leaders. Without decisive AMR can undermine decades of progress in children's health, especially in the most vulnerable regions in the world.”

